Uveitis
Know Your Eyes

Understanding Uveitis
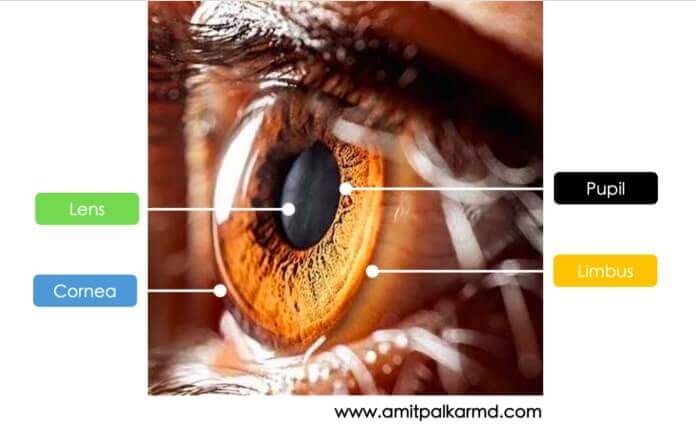
In order to understand Uveitis, lets first understand our EYE. There are 3 layers in the eye. The outer white layer that is visible to us is the Sclera. Inner to it is the middle layer of Uvea and the innermost layer is the Retina.
Uveitis occurs when the middle layer of the eyeball- Uvea gets inflamed (red and swollen). The uvea has many blood vessels that nourish the eye. Uveitis can damage vital eye tissue, leading to permanent vision loss.
Types of uveitis
There are 3 types of uveitis. They are based on which part of the uvea is affected.
Swelling of the uvea near the front of the eye is called anterior uveitis. It starts suddenly and symptoms can last many weeks. Some forms of anterior uveitis are ongoing, while others go away but keep coming back.
Swelling of the uvea in the middle of the eye is called intermediate uveitis. Symptoms can last for a few weeks to many years. This form can go through cycles of getting better, then getting worse (waxing-waning).
Swelling of the uvea toward the back of the eye is called posterior uveitis. Symptoms can develop gradually and last for many years.
In severe cases, all parts may be involved, when it is called Panuveitis.


How does a patient experience Uveitis?
Uveitis can develop suddenly. Symptoms can include:
- having a red eye with or without pain
- being very sensitive to bright light
- having blurry vision
- seeing “floaters” (specks or moving clouds in your vision) all of a sudden
Contact an ophthalmologist right away if you notice any of these symptoms.
The ophthalmologist will examine the inside of your eye. Since uveitis is often connected with other diseases or conditions, some tests may be needed. They may include a physical exam, blood or skin tests, examination of eye fluids, and imaging tests, such as X-rays. The ophthalmologist may ask about other diseases or health problems you have had. We do not always know what causes uveitis. You are more likely to get uveitis if you have or have had:
- Infections such as Tuberculosis, herpes zoster virus, herpes simplex virus, syphilis, , and parasites such as toxoplasmosis
- A systemic inflammatory disease such as inflammatory bowel disease (IBD), rheumatoid arthritis or Lupus
- An eye injury
- Smoking also increases your risk of getting uveitis.
How is Uveitis treated?
Uveitis needs to be treated right away to prevent lasting problems. Ophthalmologists often treat uveitis with eye drop medicine that reduces inflammation (corticosteroids). They may also use an eye drop to widen (dilate) the pupil, which helps reduce pain and swelling. Sometimes medicine may need to be given by injection (shots) or taken by mouth. Often times, the Uveitis specialist will work with a special kind of doctor called a Rheumatologist, or Infectious disease specialist to help treat you.
